Application development will be based on the model presented by Chavez et al. in 2019 [17] (Fig. 1). This model is a combination of iterative and incremental models in system development. According to this model, software development will be done in three different phases, which include the following:
2.1.1. Determining functional requirements
In this phase, the functional requirements of the application will be determined.
Functional requirements will be obtained through the following four methods:
-
- Selecting clinical guideline
-
- Reviewing similar studies and applications
-
- Needs assessment of patients
-
- Needs assessment and localization of requirements based on expert opinion
In this phase, based on the existing stroke self-care guidelines, one of the clinical guidelines approved by three neurologists will be selected at first and the functional requirements of this guideline will be extracted by researchers.
Other functional requirements will also be extracted using a review study on applications done by researchers and similar studies.
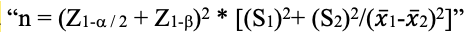
In this regard, some systematic review studies have been conducted [7, 18–21] which will also be reviewed by researchers. Needs assessment of patients will be done as the most important stakeholder group of the application. For this purpose, a semi-structured interview will be used with patients who have previously suffered from stroke and partial paralysis and have now partially recovered. These patients are required to have at least a diploma and be able to work with a smartphone. According to similar studies, participants will include three patients [22, 23] who will be selected by convenience sampling method. Finally, all these requirements will be prepared in the format of Lawshe Table and will be given to the experts. At this stage, a questionnaire containing functional requirements and information content of the application will be given to neurologists, occupational therapists and physiotherapists for the purpose of localization. Delphi technique will be used in this step. Moreover, for needs analysis, 15–21 neurologists, physiotherapists and occupational therapists who are faculty members of the country's medical universities and have at least three years of professional experience will be consulted. At this stage, for each requirement, the necessity, appropriateness, clarity and relevance will be evaluated and in terms of necessity (CVR), three levels (essential and useful, useful but unnecessary, non-useful) and in terms of appropriateness, clarity and relevance (CVI) four levels (from very high with a score of four to very low with a score of one) will be defined.
Questions with a CVR score of higher than the base number (0.62 for ten individuals) based on Lawshe table will be approved and those with a CVR score of less than that will be removed.
According to CVI, questions that have scores of higher than 0.79 will be approved and scores between 0.7 to 0.79 will be re-reviewed, corrected and returned to the experts and finally those of less than 0.7 will be rejected. This step will be repeated until the final validity of the questionnaire content is confirmed.
The approved questionnaire will be provided to the experts in the next step and the experts' answers to the components of the questionnaire will be scored from 1 to 5 (very low = 1, low = 2, medium = 3, high = 4 and very high = 5) and then the average score of each item will be calculated.
Minimum score for accepting each component will be considered as 3.75.
If the score obtained for each component is between 2.5 to 3.74, that component will be modified and reviewed again.
Components with a score of less than 2.5 will also be removed from the application content.
2.1.2. Development of low-fidelity interface
In this phase, based on the feedback and opinions received from experts in the previous step, first the items and how the application works as a conceptual model will be designed and then the low-fidelity user interface (how to display the content of the application and the relationship between humans and smartphones) on android platform will be developed using the appropriate programming language. Then, a primary prototype will be created and its validity will be evaluated. After implementing functional requirements on the prototype for checking validity, six experts will review the application and evaluate the extent to which functional requirements and goals are met by this prototype. These experts will include two neurologists, two physiotherapists and two occupational therapists with at least three years of specialized work experience in the field of treatment and rehabilitation of patients with stroke.
2.1.3. Development of high-fidelity interface
At this phase, based on the final version of the prototype obtained from the previous phase, the high-fidelity prototype will be developed.
In order to evaluate the usability of the prototype, Cognitive Walkthrough (CW) method will be used based on the method proposed by Polson and Lewis [24]. For this purpose, a certain number of scenarios that represent the most important and frequent application functions will be identified in line with the opinion of three neurologists. For each scenario, the main objective, sub-objectives, sequence of steps to do the tasks and system responses will be prepared and approved by the researchers. Then, the program will be provided to the evaluators. Five individuals will be chosen to do the evaluation through non-probability quota sampling. Evaluators are required to have at least a master's degree in health information technology/management or medical informatics and have 2 years of professional experience in evaluating health information systems. They will independently perform the sequence of steps for each scenario through the program's user interface. Each evaluator puts themselves in the position of the patient and observes the program from the patient's point of view; in case of any problems in performing task steps, it will be expressed by evaluators. This will happen at the presence of the researcher as an observer who will write the following items in data collection forms: evaluator's comments, questions and uncertainties, an explanation of the usability problem identified by the evaluator, location of the problem in the system and the time to perform each scenario. At the end of each evaluation process, each evaluator will review the list of related problems and suggest any solutions they have to solve potential issues. Then, in a meeting, separate lists of evaluators will be compared and all identified problems will be put on the list of main problems. Next, any duplicate problems will be eliminated and the evaluators will be asked to assess the severity of the problems independently. This rating will be based on three criteria including frequency of the problem, impact of the problem and continuity of the problem. Scoring for each problem and criterion will be done in 5 degrees ranging from 0 (no problem) to 4 (severe problem).
Then, the average of the identified problems will be calculated and relevant problems will be listed in order of intensity followed by feedback given to application designers.
Also, in order to confirm the application by users, the Technology Acceptance Model (TAM) will be used and Perceived Ease Of Use (PEOU), Perceived Usefulness (PU), User Satisfaction (US) and Attribute of Usability (AU) questionnaires (20 items in total) will be distributed among 30 users who have previously had a stroke and have been working with the application for a week. The results of users' comments are also given to the designers. This step will be repeated until the application is approved by evaluators. The output of this phase is the final version of the application which will be ready to be implemented in the live environment.