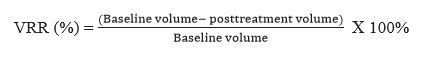
The efficacy and safety of RF ablation were demonstrated from our prospective cohort single-center study which was performed by only one endocrinologist with 3 years of experience. Only two cases (2.56%) with transient voice change occurred on 78 patients in 2 years of study and no major complication was found. Thyroid functions were constant after 1- month post-ablation. Regarding efficacy, RFA reduced nodule volume by 41.47%, 64.72% after 1 and 3 months post-ablation, respectively. This represents approximately 30.8% and 84.6% therapeutic success rates in this follow-up period. In addition, patients who were treated by RFA improved their symptom score and cosmetic score significantly. We found that only characteristics of nodules significantly related to the VRR during the 3 months follow-up.
Benign thyroid nodule(s) is a relatively common disease. Its traditional treatment options include surgery, T4 suppressive therapy. However, both of them had some limitations. Radiofrequency ablation has been adopted worldwide as a minimally invasive treatment of benign thyroid nodules. It has proven to be a safe and effective option but the results have been heterogeneous in many studies. The VRR ranged from 32.7–58.2% at 1 month [22–24]; 50–85.5% after 3 months depending on different ablation machine systems, basic techniques, and thyroid nodule’s characteristics in the studies [25–27]. Our study showed suitability in VRR results during the 1 month and 3 months follow-up, matched with the literature. A gradual progression of VRR, which was approximately 44.6–84.1% at 6 months; 58–89.6% at 12 months; 84–88% at 2 years was showed in many longer follow-up studies [25, 28–33]. The quick decrease of nodule volume within 3 months post-ablation helps to improve the symptomatic and cosmetic problems.
The safety profile of thyroid RFA was demonstrated in the literature. In treating benign thyroid nodules, the prevalence of RFA complications was 2.11% for overall complications, and 1.27% for major complications [34–36]. No major complications were found in our study and 2.56% of minor complication (transient voice change) occurred. It’s all because of strictly applying two fundamental techniques (the moving-shot technique and the trans-isthmic approach) during the RFA procedure. These techniques help to not only prevent hot fluid escape and the electrode tip changing in the position when patients talk, swallow, or cough but also limiting damage to surrounding tissue [12, 19]. Moreover, in a few cases to preventing important structures such as nerves and arteries when complete ablation of the nodule with unfavorable anatomy was desired, the hydro-dissection technique was used by injecting slowly 5% dextrose. For management of voice change after RFA, we injected cold 5% dextrose (0°C to 4°C) as the same hydro-dissection technique [37]. In addition, our study showed thyroid function test was no change. These results agree with some study conclusions that the rate of hypothyroidism and hypoparathyroidism were reduced as compared to surgery.
In many previous studies, factors such as initial volume, the solidity of the nodule, vascularity, applied energy, and initial ablation ratio was related to the efficacy of RFA for thyroid nodules (VRR) [13–18]. In agreement with previous findings, our study confirmed only internal component of nodules as an independent factor affecting the VRR. Higher VRR occurred in cystic or predominantly cystic nodules. The cystic fluid of the nodule was aspirated before the RFA procedure followed by a quick reduction in the volume of the ablated nodule. Also, due to solid components and their vascularity which secrete the fluid were ablated, the recurrence of a cystic nodule was effectively prevented. However, our results showed no association between other factors (baseline characteristics of the patients and nodules, treatment characteristics) and the VRR. Sim and et al show that the IAR is a factor highly correlated with the VRR. If the IAR is greater than 70% and the VRR greater than 50%, therapeutic success may be expected after RFA [18].
Our study has several limitations. Firstly, the follow-up in this prospective study was largely affected by irregular patient’s follow-up intervals during the COVID19 pandemic. A single-center study with relatively small sample size and short time follow-up of 1 month, 3 months is another limitation. Some variables include vascularity of nodule and IAR were not collected. These limitations inspire our group to do larger and longer prospective multicenter cohort studies to prove these results.
In conclusion, RFA was demonstrated as a safe and effective option for benign thyroid nodules treatment. The VRR reached 41.47%, 64.72% after 1 and 3 months post-ablation. Minor complication (transient voice change) occurred in two cases after the RFA procedure and thyroid functions were constant. We found only the internal component of nodules as an independent factor affecting the VRR during the 3 months follow-up. Thus, RFA can be used as an alternative treatment with encouraging results, fewer complications.